In today’s healthcare landscape, multi-specialty practices are increasingly common, blending diverse medical disciplines under one roof to offer comprehensive care. However, the complexity of managing billing and coding for various specialties can be daunting. Each specialty has its own unique codes, regulations, and payer requirements. For healthcare providers, having an efficient and specialized billing and coding system is essential to prevent revenue loss, streamline claims processing, and ensure compliance. This guide provides an in-depth look at multi-specialty billing and coding, outlining best practices, challenges, and benefits.
Understanding Multi-specialty Billing and Coding
Multi-specialty billing and coding involve handling claims and documentation for practices that offer more than one type of medical service, such as cardiology, orthopedics, neurology, and internal medicine. Each specialty has unique billing requirements, making it necessary to understand the intricacies of coding for each one. Accurate coding is vital as it directly affects reimbursement rates, compliance with regulations, and timely payment from payers.
The primary focus of multi-specialty billing is to create a streamlined process where each department’s unique requirements are met without compromising the speed and accuracy of claims submission. This involves staying up-to-date on the latest coding changes for each specialty, understanding payer-specific rules, and ensuring all documentation supports the billed codes.
Key Challenges in Multi-specialty Billing and Coding
Multi-specialty billing presents several challenges, primarily due to the range of codes and payer requirements. Here are some of the common issues faced by billing professionals:
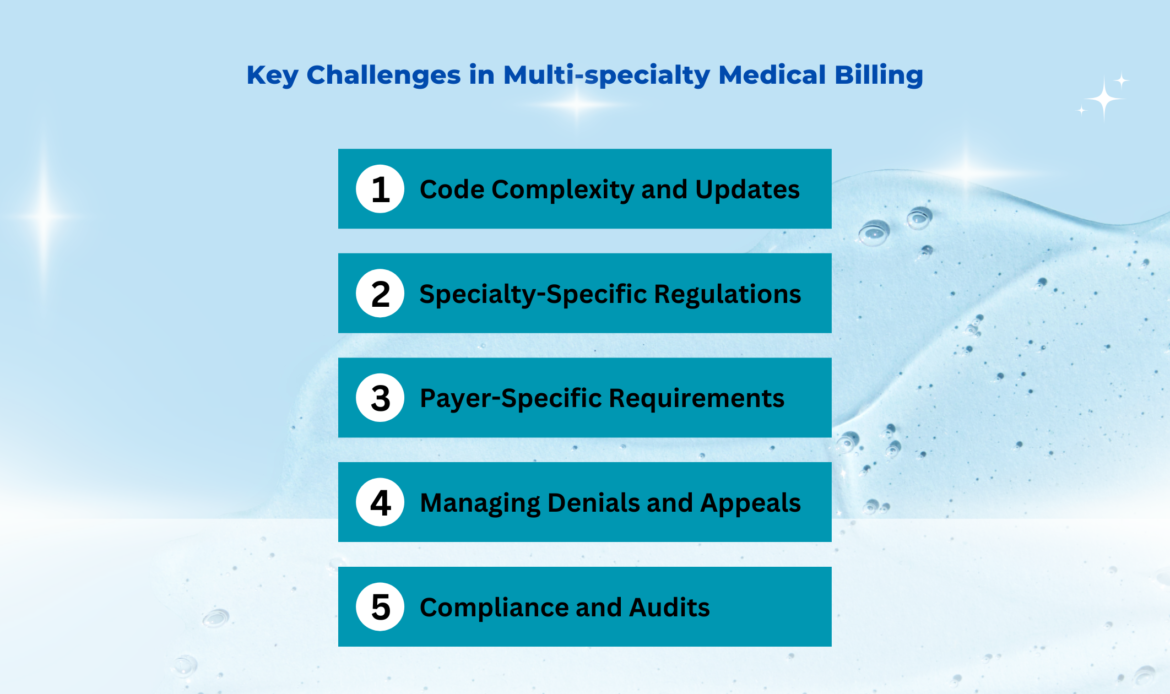
- Code Complexity and Updates: Each specialty has its own set of Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes. Managing the frequent updates to these codes and staying compliant requires ongoing education and training.
- Specialty-Specific Regulations: Certain specialties, such as cardiology or orthopedics, may have specific coding rules, such as modifiers for surgeries or procedures. Misinterpreting these guidelines can result in denials or underpayments.
- Payer-Specific Requirements: Insurance companies often have their own rules regarding documentation, coding, and claims submission. Understanding and adapting to these requirements across multiple payers can be challenging.
- Managing Denials and Appeals: Denials are more common in multi-specialty practices due to the range of services provided. Effective denial management involves quick identification of the reason for denial, appeals processes, and resubmission strategies.
- Compliance and Audits: Ensuring that all billing practices comply with federal and state regulations is essential to avoid penalties. Practices with multiple specialties are more likely to be audited, making compliance a top priority.
Best Practices for Multi-specialty Billing and Coding
Multi-specialty billing requires a well-coordinated approach to maintain accuracy and efficiency. Here are some key practices that can help manage this complexity effectively:
- Specialized Training: Billing staff should be trained in the nuances of each specialty they handle. This includes understanding specialty-specific codes, modifiers, and common procedures. Continuous education is essential to keep up with changing regulations and code updates.
- Advanced Coding Software: Leveraging specialized coding software that can handle the demands of multi-specialty billing is crucial. The software should allow for code specificity, compliance checks, and real-time updates on coding changes.
- Efficient Denial Management: Creating a proactive system for managing denials is essential. Regular analysis of denial patterns can help identify problem areas, allowing billing staff to make necessary adjustments and reduce future denials.
- Compliance Monitoring: To mitigate the risk of audits, it’s important to implement a compliance program that regularly reviews billing practices and ensures they align with payer requirements and federal regulations.
- Clear Documentation Practices: Accurate and detailed documentation is the backbone of successful billing. Each specialty must document services thoroughly to support the codes billed, helping reduce errors and improve claim approval rates.
- Effective Communication Between Departments: Coordinating across different specialties requires clear communication to ensure accurate billing. Regular meetings or digital collaboration tools can help synchronize efforts between clinical and billing departments.
Medical Billing Specialties We Serve
At MediBill Health Partners, we specialize in managing the unique billing and coding requirements across a variety of medical fields. Our team is dedicated to providing precise, compliant, and efficient billing support for each specialty we serve, ensuring practices can maximize revenue and focus on patient care. Here are some of the specialties we proudly support:
- Podiatry: Our podiatry billing team expertly navigates Medicare regulations and codes for foot and ankle treatments, optimizing reimbursements and reducing claim denials.
- Neurology and Neurosurgery: We handle complex neurology billing with certified coders who are knowledgeable in payer requirements, helping to reduce denials and streamline cash flow.
- Internal Medicine: Our internal medicine billing services cover everything from coding and claims submission to collections, so providers can concentrate on patient care.
- Behavioral and Mental Health: We understand the specific documentation and compliance needs of behavioral health services, ensuring claims are processed accurately and promptly.
- Wound Care: Our wound care billing covers specialized areas such as burn care, diabetic wound care, and post-surgical management, ensuring accuracy and efficiency in claims.
- Long-term Nursing Care: We manage billing for daily rates and ancillary services, tailoring our approach to meet the needs of long-term care facilities and improve reimbursement cycles.
- Chiropractic Care: Our chiropractic billing team is skilled in handling the unique documentation and coding requirements for spinal adjustments, therapeutic exercises, and other chiropractic services, ensuring providers receive timely reimbursements.
- Pediatrics: For pediatric practices, we manage complex billing requirements, including vaccinations, developmental screenings, and specialized treatments, to support a smooth billing cycle and optimize revenue.
- Family Medicine: Our family medicine billing solutions cover a broad range of services, from routine check-ups to chronic disease management, with a focus on accuracy and compliance for each family-focused visit.
- Laboratory Billing: We specialize in laboratory billing for diagnostic tests, pathology, and other lab services, ensuring accurate coding and compliance to support timely reimbursements.
- General Practice: Our billing team supports general practitioners by managing a variety of services, from preventative care to acute treatment, streamlining the process and improving cash flow.
By providing expertise in each of these specialties, MediBill Health Partners ensures accurate billing and coding, reduces administrative burdens, and supports a seamless revenue cycle for multi-specialty practices. With our support, healthcare providers can trust that each specialty’s unique needs are met, maximizing reimbursements and allowing them to prioritize patient care.
How Our RCM Works?
Our Revenue Cycle Management (RCM) process at MediBill Health Partners is designed to ensure smooth, efficient, and accurate billing from the initial patient encounter through payment collection. By focusing on every stage of the revenue cycle, we help practices maximize their reimbursements and minimize claim denials. Here’s a breakdown of each step in our RCM process:
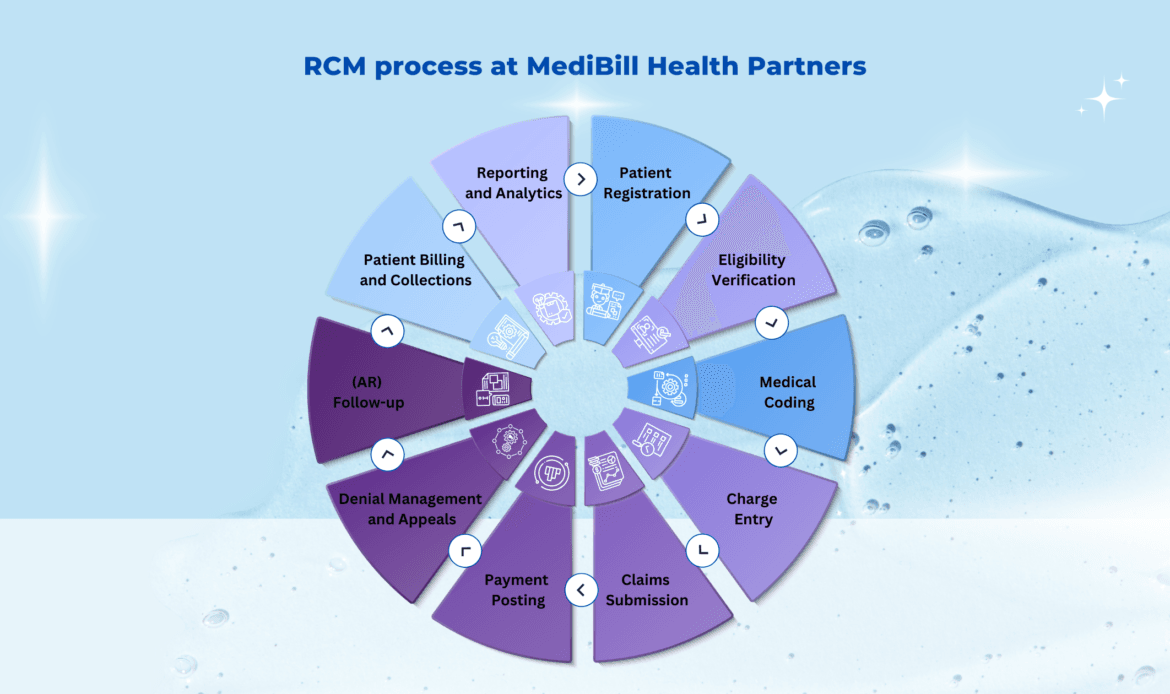
- Patient Registration and Eligibility Verification: We start by gathering all relevant patient information, including demographics and insurance details. Our team verifies insurance eligibility and benefits before services are provided, ensuring that all information is accurate and up-to-date to prevent potential issues later in the billing process.
- Medical Coding: Our certified coders translate patient diagnoses, procedures, and treatments into accurate CPT, ICD-10, and HCPCS codes. Each specialty’s specific coding requirements are carefully followed to avoid errors and ensure compliance with payer guidelines, which helps maximize reimbursement rates.
- Charge Entry: We input all coding and charges into the billing system, ensuring that each service rendered is correctly documented. This step involves a meticulous review to confirm that the charges accurately reflect the procedures performed, creating a clear and complete record for each patient visit.
- Claims Submission: Our team prepares and submits claims electronically to the respective payers, following each payer’s unique submission requirements. We prioritize submitting clean claims on the first attempt, reducing the likelihood of rejections and delays in payment.
- Payment Posting: Once payments are received from payers, our team posts them accurately to the respective accounts. We also handle any adjustments and deductibles, ensuring that the payment posting aligns with the Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) details.
- Denial Management and Appeals: If claims are denied or rejected, we promptly identify the cause, whether it’s coding discrepancies, documentation issues, or payer-specific requirements. Our team corrects the errors, resubmits the claim, or initiates an appeal if necessary, to recover the maximum reimbursement.
- Accounts Receivable (AR) Follow-up: Our dedicated AR specialists monitor outstanding claims and follow up with payers to ensure timely payment. We focus on reducing aging AR by regularly tracking unpaid claims, identifying patterns in delays, and pursuing payment with persistence to improve cash flow.
- Patient Billing and Collections: For balances owed by patients, we handle billing statements and communicate with patients regarding their responsibility for payment. Our team ensures transparency and clarity in patient billing, facilitating a smoother collection process and enhancing patient satisfaction.
- Reporting and Analytics: Throughout the process, we provide detailed reporting and analytics to help practices understand their financial performance. Our reports include insights on reimbursement rates, claim denials, payment trends, and AR days, allowing providers to make informed decisions and optimize their revenue cycle.
Each of these steps is tailored to fit the unique needs of the specialty, ensuring that every aspect of the billing cycle is managed with accuracy and efficiency. By following a structured approach to RCM, MediBill Health Partners enables practices to maximize revenue, reduce administrative burdens, and focus on delivering quality patient care.
Benefits of Partnering with a Multi-specialty Billing and Coding Service
For many practices, partnering with a specialized billing and coding service can streamline operations, reduce errors, and improve cash flow. Here are some key benefits of outsourcing multi-specialty billing:
- Expertise Across Specialties: A specialized billing service provides access to a team with expertise in multiple specialties, ensuring each area receives the necessary focus and knowledge for accurate coding.
- Improved Cash Flow: By minimizing denials and optimizing coding accuracy, specialized billing services help practices receive reimbursements faster and reduce delays in revenue.
- Reduced Administrative Burden: Outsourcing allows healthcare providers to focus on patient care rather than dealing with billing complexities. This leads to higher efficiency in practice management and better patient outcomes.
- Compliance and Risk Management: Specialized billing services are well-versed in compliance requirements and can ensure that all billing practices meet regulatory standards, reducing the risk of audits and penalties.
- Access to Advanced Technology: Many billing services use cutting-edge software to streamline billing operations. This technology enables real-time tracking, compliance checks, and efficient claims submission across multiple specialties.
Conclusion
Multi-specialty medical billing and coding is essential to maximizing revenue for healthcare practices that offer diverse services. While it comes with unique challenges, implementing best practices and utilizing specialized services can streamline the process, reduce errors, and enhance financial outcomes. By understanding the complexities of each specialty’s billing needs and leveraging professional support, practices can ensure compliance, reduce administrative burdens, and focus more effectively on patient care.

