In the complex world of healthcare, efficient billing and revenue cycle management are essential for any practice to thrive. One of the most critical, yet often overlooked, aspects of this system is credentialing and enrollment. Credentialing and enrollment not only ensure that healthcare providers meet necessary qualifications but also that they are authorized to receive reimbursement from insurance companies and other payers.
At MediBill Health Partners, we recognize how crucial this process is and aim to help medical practices streamline their credentialing and enrollment for smoother operations and faster reimbursement. Let’s dive deeper into what credentialing and enrollment entail, why they are indispensable to the success of your practice, and the step-by-step process of credentialing.
Understanding Credentialing and Enrollment:
Before a healthcare provider can see patients and get reimbursed for their services, they must go through the credentialing and enrollment process. Both terms are sometimes used interchangeably, but they refer to different stages in the process.
Credentialing
Credentialing is the process through which a healthcare provider’s qualifications are verified. This ensures that providers meet the required educational, training, licensing, and professional standards to deliver medical care. Credentialing also involves reviewing a provider’s background, including their work history, malpractice history, certifications, and licenses.
Enrollment
Once the credentialing process is complete, the provider moves on to the enrollment phase. Enrollment refers to the process of registering a provider with insurance networks, government programs (like Medicare and Medicaid), and other third-party payers. Successful enrollment allows healthcare providers to bill these entities for the services they provide to patients.
Without proper enrollment, even the most qualified healthcare provider may face delayed payments, denied claims, or, worse, the inability to serve patients under certain insurance plans. Thus, credentialing and enrollment go hand-in-hand to ensure smooth operations and proper reimbursement in a healthcare practice.
Who Verifies Credentials?
The credentialing process involves multiple parties responsible for verifying a healthcare provider’s qualifications and background. Here’s a closer look at who conducts these verifications:
- Insurance Companies: Private and commercial insurance companies verify the credentials of healthcare providers before allowing them to enroll in their networks. These companies rely on primary source verification to ensure providers meet specific standards and regulations.
- Credentialing Organizations: Third-party credentialing verification organizations (CVOs) are often contracted by insurance networks, hospitals, or healthcare practices to handle the credentialing process. These organizations specialize in gathering and verifying provider information from reliable primary sources.
- Hospitals and Healthcare Networks: For providers seeking hospital privileges or to join a healthcare network, the hospital’s credentialing committee performs the verification process. This committee is responsible for reviewing education, training, and professional history to approve the provider for practice.
- Government Payers: Medicare and Medicaid also conduct their own credentialing processes to ensure providers meet federal and state-level requirements before enrollment in their programs.
What is a Credentialing Checklist?
A credentialing checklist is a comprehensive list of required documents and information that healthcare providers must submit during the credentialing process. Having this checklist prepared ensures that all necessary items are provided to avoid delays in the application process. Here’s a general breakdown of what a typical credentialing checklist might include:
- Personal Information
- Educational Background
- Professional Licenses and Certifications
- Work History and Experience
- Malpractice Insurance Coverage
- Professional References
- Criminal Background and Disciplinary History
- Continuing Medical Education (CME)
- Hospital Privileges
- NPI Number
This checklist helps providers stay organized and ensures that all necessary documentation is in place, reducing the chances of missing information and delays in the credentialing process.
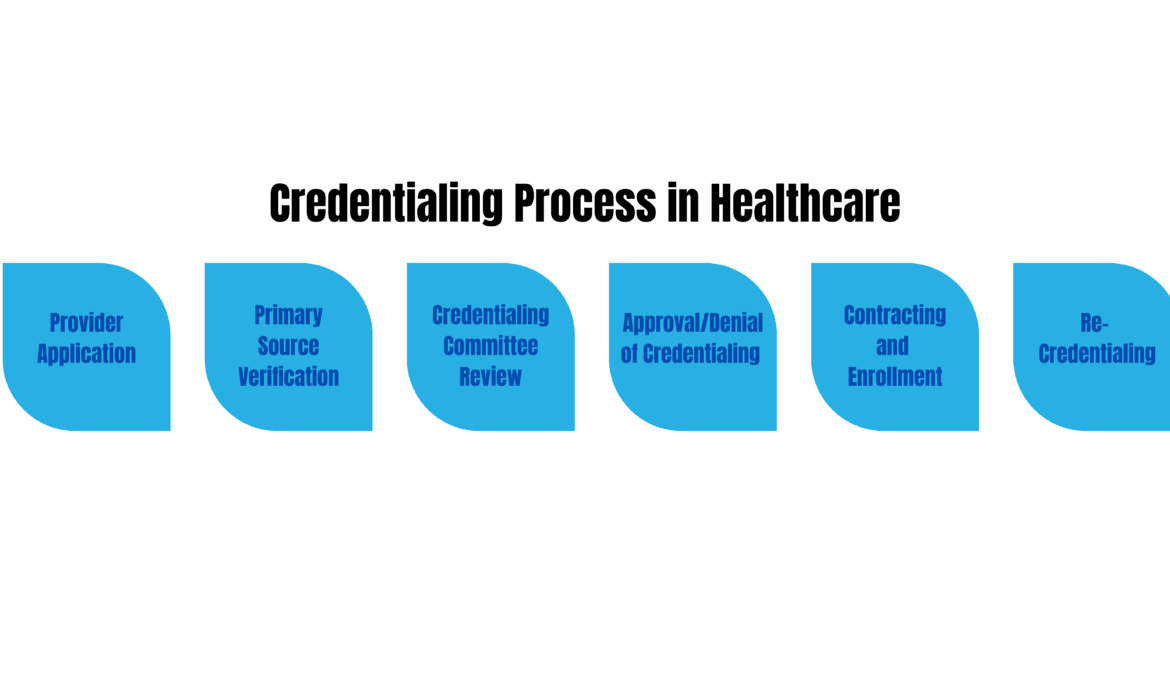
The Credentialing Process: Step by Step:
Credentialing can be a complex process, but understanding each step will help medical practices prepare and navigate it efficiently. Here’s a clear breakdown of the typical steps involved in credentialing:
- Application Submission
The first step is filling out and submitting a credentialing application to the payer or credentialing organization. This application requires detailed information about the provider’s education, training, experience, and licensure. It also typically asks for documents like diplomas, state licenses, DEA certification, and board certifications. At MediBill Health Partners, we assist in compiling and submitting this critical documentation, ensuring that no details are overlooked. - Primary Source Verification (PSV)
Once the application is submitted, the payer or credentialing organization will begin verifying the accuracy of the information provided. This process, known as Primary Source Verification (PSV), involves contacting educational institutions, licensing boards, and previous employers to confirm the provider’s credentials. The verification process can take time, so ensuring that all information submitted is correct and up-to-date can help prevent unnecessary delays. - Background and Professional History Check
In addition to verifying education and licenses, credentialing organizations conduct thorough background checks. These reviews look into the provider’s criminal history, malpractice claims, and any professional disciplinary actions. Providers with issues in their background may face additional scrutiny, but full transparency at this stage is essential for moving forward in the process. - Review by Credentialing Committee
After completing the verification and background check, the payer or organization will present the application and findings to a credentialing committee. This committee typically consists of medical professionals and administrative personnel who review the provider’s qualifications to ensure they meet the required standards. If everything is in order, the committee approves the application, allowing the provider to move on to enrollment. - Approval and Notification
Once the credentialing committee gives its approval, the payer or credentialing organization will notify the healthcare provider and the practice of the decision. If any additional steps or documents are required, they will request them at this stage. Upon approval, the provider is officially credentialed, and their information will be stored in the payer’s database for future reference. - Recredentialing and Ongoing Maintenance
Credentialing is not a one-time task. Providers must undergo recredentialing at regular intervals (often every two to three years) to ensure that they continue to meet all qualifications and standards. Additionally, any changes in the provider’s credentials (such as new licenses, certifications, or employment) must be updated with the credentialing organization to maintain compliance.
The Importance of Credentialing and Enrollment for Your Practice:
The credentialing and enrollment process is not just an administrative formality; it’s an essential function that has a direct impact on the financial health of a practice. Here’s why getting it right is critical:
- Ensures Timely Reimbursement
Credentialing and enrollment are the gatekeepers to getting paid. If a provider is not credentialed or enrolled with payers, they cannot submit claims or receive reimbursement for the services they provide. Delays or errors in the process can lead to significant revenue losses and create a financial strain on your practice.
- Boosts Patient Trust and Satisfaction
Patients want to feel secure that they are receiving care from qualified professionals. Credentialing offers that assurance, as it confirms a provider’s qualifications and experience. Furthermore, enrollment in various insurance networks ensures that patients can access care using their insurance plans, leading to higher patient satisfaction and retention.
- Expands Patient Base
When a healthcare provider is enrolled with multiple insurance companies, they have the opportunity to see a larger pool of patients. This increases the practice’s reach, bringing in more patients and subsequently more revenue. Practices that fail to enroll their providers with a wide array of payers may inadvertently limit their growth potential.
- Minimizes Legal and Compliance Risks
Healthcare is heavily regulated, and improper credentialing and enrollment can expose a practice to legal issues, fines, or penalties. Staying compliant with payer requirements helps avoid these risks. Additionally, it ensures that the practice is always operating within the confines of the law, which protects both the provider and the patients.
Challenges in Credentialing and Enrollment:
While credentialing and enrollment are necessary processes, they can often be complicated, time-consuming, and prone to delays if not managed efficiently. Some common challenges include:
- Extensive Documentation Requirements
The credentialing process involves gathering and verifying a large amount of information, including education, certifications, licenses, and work history. Missing or outdated documents can cause significant delays.
- Changing Payer Requirements
Payers often update their requirements for provider credentialing and enrollment, which means practices need to stay up-to-date to avoid costly delays. Missing a payer’s new criteria could mean denial of claims or lost revenue.
- Lengthy Processing Times
Credentialing and enrollment are notoriously slow processes. It can take anywhere from 60 to 120 days, or even longer in some cases, for a provider to become fully credentialed and enrolled. Practices that don’t anticipate these timelines can experience financial shortfalls as they wait to bill for services.
- Inconsistent Communication with Payers
Practices may experience poor communication with insurance companies during the credentialing and enrollment process. This can result in missed deadlines, additional documentation requests, or extended waiting periods, further delaying the start of billing and reimbursement.
MediBill Health Partners’ Credentialing and Enrollment Solutions:
At MediBill Health Partners, we understand the complexities involved in credentialing and enrollment, which is why we offer specialized services to take the burden off your practice’s shoulders. Our expert team manages the entire process from start to finish, ensuring that your providers are credentialed and enrolled efficiently and effectively. Here’s what sets us apart:
- Expertise in Healthcare Credentialing
Our dedicated credentialing team has years of experience working with healthcare providers and payers. We stay updated on the latest payer requirements and regulations to ensure a smooth process.
- Thorough Document Management
We manage and verify all required documents, from education and certifications to work history and licensing, ensuring nothing is missed. This minimizes the risk of delays or denied enrollments.
- Proactive Communication
We maintain close communication with insurance companies and payers throughout the credentialing and enrollment process. This helps avoid any miscommunication, errors, or unnecessary delays, allowing your practice to get credentialed and enrolled in the shortest time possible.
- Ongoing Maintenance
Credentialing and enrollment aren’t one-time tasks. Providers must continually maintain their status with payers by keeping their information updated. MediBill Health Partners offers ongoing monitoring to ensure that your providers remain compliant and credentialed, avoiding any disruptions to your revenue stream.
Conclusion
Credentialing and enrollment are vital components of any healthcare practice’s operational success. These processes ensure that healthcare providers are qualified to deliver care and that they can bill insurance companies and other payers for their services. Without proper credentialing and enrollment, practices risk delayed payments, denied claims, and even legal issues.
At MediBill Health Partners, we specialize in simplifying the credentialing and enrollment process, allowing healthcare providers to focus on what matters most—delivering quality care to patients. With our expertise, proactive approach, and commitment to minimizing delays, we help practices maximize their reimbursement potential and avoid administrative headaches.
If you’re looking to streamline your credentialing and enrollment process, reach out to MediBill Health Partners today and let us take care of the heavy lifting.
More info: