In the ever-evolving healthcare landscape, understanding administrative and regulatory terms is not just important — it’s essential. Two of the most commonly misunderstood concepts are credentialing and privileging. Although both are critical for healthcare operations, they serve very different functions and impact healthcare delivery at multiple levels.
At MediBill Health Partners, we specialize in helping providers and healthcare organizations stay compliant, efficient, and informed. In this guide, we’ll explore the detailed differences, procedures, and regulations surrounding credentialing and privileging — and why both are vital to your organization’s success.
What is Credentialing?
Credentialing is the foundational process of verifying that healthcare professionals possess the necessary qualifications, training, and legal permission to provide care. This isn’t just a one-time verification — it’s a formal, standardized, and ongoing process that ensures only properly educated and trained individuals are allowed to practice in clinical environments.
Credentialing is usually required before a provider can:
- Join a medical group or hospital staff
- Be reimbursed by insurance companies (including Medicare & Medicaid)
- Sign contracts with payers or facilities
- Deliver services under an organization’s name
The Core Objectives of Credentialing
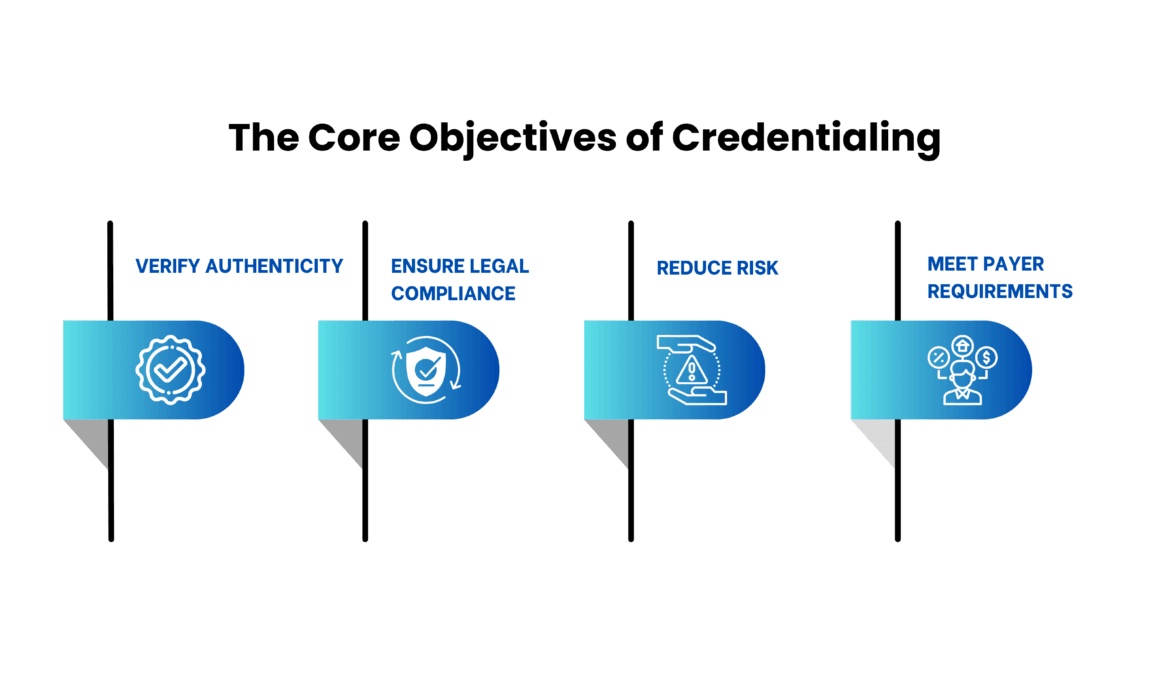
- Verify Authenticity: Confirm that degrees, licenses, and certifications are legitimate and up to date.
- Ensure Legal Compliance: Verify that providers meet all legal requirements to practice.
- Reduce Risk: Minimize the chances of patient harm, malpractice, or fraud.
- Meet Payer Requirements: Insurance companies won’t process claims from uncredentialed providers.
The Credentialing Process: Step-by-Step
- Collection of Documentation
Providers submit diplomas, state licenses, board certifications, DEA registrations, malpractice insurance, and professional references. - Primary Source Verification (PSV)
Institutions verify each credential by contacting the original source — like the medical school or licensing board — rather than accepting submitted copies at face value. - Licensure and Sanction Checks
Providers are checked against federal and state databases to ensure their license is active and that they have no history of disciplinary action. - Review of Clinical History
Work history is evaluated for gaps, red flags, or employment at institutions with known compliance issues. - Background Checks
Criminal records, civil judgments, drug screenings, and malpractice claims history are all reviewed. - Credentialing Committee Review
A designated body within the healthcare facility reviews the verified information and approves or denies affiliation. - Re-Credentialing
Credentialing is not permanent. CMS and most commercial payers require re-credentialing every 2 to 3 years.
CMS Credentialing Requirements
The Centers for Medicare & Medicaid Services (CMS) outlines detailed credentialing standards under its Conditions of Participation (CoPs) and Conditions for Coverage (CfCs). Compliance is not optional if a facility wants to participate in federal programs.
Key CMS mandates include:
- Primary Source Verification (PSV): Credentials must be verified directly from issuing organizations.
- Regular Reassessment: Practitioners must be reviewed periodically for continued compliance.
- NPDB Checks: The National Practitioner Data Bank must be queried to assess malpractice, license restrictions, or fraud issues.
- Policy Governance: A facility must have documented policies, procedures, and a credentialing committee in place.
- Legal & Ethical Compliance: Credentialing must comply with HIPAA, state practice laws, and other healthcare regulations.
What is Privileging?
While credentialing validates a provider’s ability to practice medicine, privileging determines what specific services or procedures a provider is authorized to perform within a particular facility.
Privileging is institution-specific. For example, just because a physician is licensed and board-certified doesn’t automatically mean they can perform surgeries at any hospital. The hospital must first assess and approve the provider’s qualifications for specific roles or tasks.

Real-World Example of Privileging
A general surgeon might be credentialed and licensed in the state. However, to perform laparoscopic bariatric surgeries at a specific hospital, they must submit additional proof of:
- Specific training in laparoscopic techniques
- Experience in similar surgeries
- Successful case outcomes
- Peer reviews or mentorship letters
- Ongoing continuing medical education (CME) in that specialty
Only after passing this evaluation will the hospital grant surgical privileges for that specific procedure.
The Privileging Process: Step-by-Step
- Privilege Application
The provider requests privileges for specific services or procedures and submits evidence of relevant training, case logs, and CME credits. - Assessment of Clinical Competence
The facility reviews the provider’s qualifications in relation to the requested privileges. This might include simulation-based evaluations, observed procedures, or review of outcomes. - Peer Review & Reference Checks
Input from other specialists in the same field is obtained. Feedback may come from past supervisors or colleagues. - Medical Staff Review
The medical staff office or credentialing committee uses bylaws and policies to determine whether to grant the requested privileges. - Granting of Privileges
If approved, privileges are defined, documented, and limited to what was requested and verified. - Ongoing Competency Review
Hospitals review provider performance regularly, typically every 12 to 24 months, before renewing privileges.
CMS Privileging Guidelines
CMS defines specific requirements for privileging under the Medical Staff and Governing Body Conditions of Participation. These focus heavily on accountability, fairness, and provider competence.
Highlights include:
- Medical Staff Bylaws Must Define Privileging Criteria: Facilities must have clear, documented guidelines to assess which providers can do what.
- Competence Over Credentials: Decisions should prioritize demonstrated ability, not just academic qualifications or professional memberships.
- Institutional Autonomy: Facilities must retain control over privileging decisions — no external certification or society membership should dictate authority.
Why Credentialing & Privileging Matter
These processes aren’t just regulatory checkboxes — they form the core of safe, ethical, and legal healthcare delivery. When done correctly, they benefit everyone: patients, providers, payers, and institutions.
- Ensures Patient Safety
Thorough vetting helps prevent unqualified individuals from treating patients, minimizing risks of misdiagnosis, errors, or complications. - Reduces Legal Liability
Proper credentialing and privileging offer a legal defense in cases of malpractice by proving the organization acted responsibly in vetting providers. - Protects Facility Accreditation
Failing to meet CMS or Joint Commission requirements for credentialing and privileging can result in lost reimbursement eligibility or facility shutdowns. - Promotes Professional Excellence
Credentialing and privileging encourage ongoing education, training, and performance improvement — benefitting both providers and patients. - Streamlines Revenue Cycle
Payers require credentialed providers for claim approval. Incomplete or outdated credentialing can result in delayed payments or denials. - Builds Trust
Patients are more confident in their care when they know their providers have been thoroughly vetted and approved by their healthcare facility.
Credentialing vs Privileging: Side-by-Side Comparison
| Feature | Credentialing | Privileging |
|---|---|---|
| Goal | Validate qualifications to legally practice | Grant specific permission to perform procedures or offer services |
| Scope | Licensure, education, training, background, sanctions | Clinical skills, experience, observed competence |
| Who Does It | Credentialing office, HR, compliance committee | Medical staff office, clinical leadership, peer reviewers |
| When Conducted | At time of hire or enrollment with payers; every 2-3 years thereafter | Upon onboarding and when applying for new roles or services; renewed every 1-2 yrs |
| Governing Regulations | CMS CoPs, NCQA, payer requirements, state boards | CMS CoPs (Medical Staff & Governing Body), hospital bylaws |
| Outcome | Eligibility to work or bill as a provider | Authorization to perform clinical procedures or services within facility |
Let MediBill Health Partners Handle Your Credentialing Needs
Credentialing can be a time-consuming, frustrating process. Missing even one detail can delay reimbursements or cause compliance issues. That’s where MediBill Health Partners comes in.
We offer end-to-end credentialing services, including:
- Document collection and verification
- Payer enrollment and revalidation
- Compliance with CMS, NCQA, and state-specific regulations
- Monitoring for expiring licenses and certifications
- Privileging support for hospital or facility onboarding
Let us manage the paperwork, timelines, and regulations — so you can focus on delivering exceptional care.
📞 Ready to simplify your credentialing process?
Contact MediBill Health Partners today for a free consultation. (Credential with confidence. Practice with purpose.)

